Contributing physicians in this story

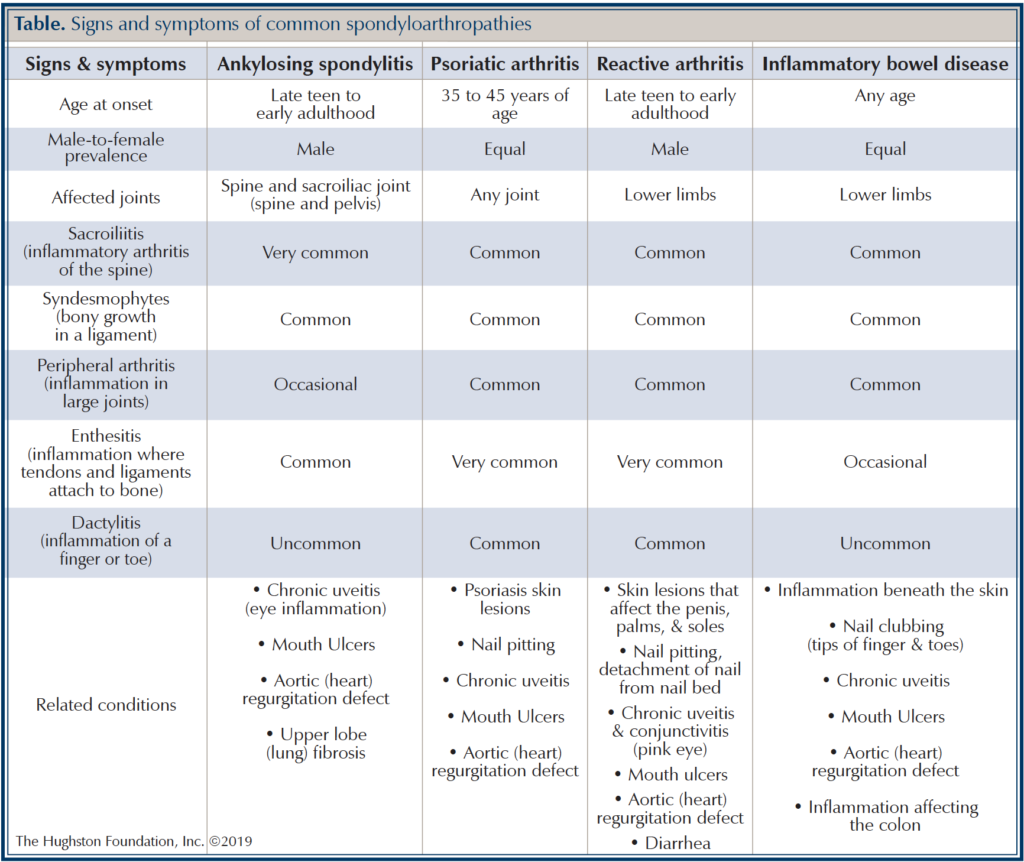
Spondyloarthropathies are a group of chronic (long term) inflammatory diseases, often referred to as spondyloarthritis, which damage various joints throughout your body. These diseases include ankylosing spondylitis (AS), psoriatic arthritis, reactive arthritis, and arthritis associated with inflammatory bowel disease (Table). Seen in both children and adults, widespread inflammation— classic signs are heat, redness, swelling, pain, and loss of function—often cause low back pain, morning stiffness, and fatigue. Although they have similar symptoms, spondyloarthropathies are different from rheumatoid arthritis in adults and juvenile idiopathic arthritis in children. If you have a form of spondyloarthropathy, depending on the type, it can affect your skin, nails, intestines, heart, spine, and eyes in addition to your joints.
Who is at risk?
Spondyloarthritis often affects males in their teens or 20s and for some patients, it may run in families. Researchers have identified the HLA-B27 gene as a cause for ankylosing spondyloarthritis; however, there are as many as 30 other genes linked to different types of spondyloarthropathies. Not everyone who carries the HLA-B27 gene develops arthritis; still, since there is a genetic link associated with these diseases, family members of affected individuals are at higher risk.
Symptoms
The location of inflammation or concomitant disease (related conditions) is specific to each type of spondyloarthropathy, but all have an overlap of symptoms (see table). For instance, ankylosing spondylitis (AS) will commonly affect the sacroiliac joints (joint between the spine and pelvis) and spine. This type can affect your other joints, such as your knees, but the SI joints are specific to AS. Psoriatic arthritis will affect the knees, hips, spine, and classically the hands and fingers. Skin and nail changes will occur alongside the inflammation of joints. Reactive arthritis, also known as Reiter’s syndrome, is an inflammatory arthritis often triggered by a bacterial infection. It generally begins several weeks after a urinary and gastrointestinal tract infection. Arthritis associated with inflammatory bowel disease has symptoms similar to the other spondyloarthropathies but is associated with Crohn’s disease or ulcerative colitis. Chronic inflammation can occur if the inflammation goes untreated resulting in destructive changes to the joints that then become evident on x-ray. These are only some of the changes as these diseases result in wide-spread inflammation and can involve heart, lungs, kidneys, and the gastrointestinal tract.
Diagnosing spondyloarthropathies
To diagnose the disease, your physician will complete a thorough physical exam and an in-depth health history. Patients diagnosed with one of the spondyloarthropathies will generally have some combination of joint pain and other extra-articular (outside the joint) symptoms ranging from skin changes (psoriatic arthritis), urinary tract infection (reactive arthritis), to bowel complications including diarrhea or constipation (Crohn’s disease/ulcerative colitis associated arthritis). Once your physician suspects spondyloarthropathy based on your family history, health history, and physical examination, he or she may order lab testing to confirm the diagnosis.
Treatment
Spondyloarthropathies are diseases of inflammation; therefore, anti-inflammatory medications are the cornerstone of treatment. Medications prescribed generally begin with over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen or your doctor can prescribe a stronger prescription NSAID if needed. If you do not respond to NSAIDs, your doctor can prescribe medications known as disease modifying antirheumatic drugs (DMARDs), such as sulfasalazine (Azulfidine®), methotrexate (Rheumatrex®), etanercept (Enbrel®) or infliximab (Remicade®). These drugs, in one way or another, decrease the inflammation in the body. If the effect of chronic inflammation results in end-stage arthritis, your physician may recommend surgical management for your symptoms. With the advent of the DMARDs, joint destruction and the ill effects of chronic inflammation has lessened the need for early surgical management.
In addition to medications, your doctor will also recommend nonpharmacologic modalities, which can include physical therapy and home exercise and stretching programs. Your physician may recommend that you become more active by taking up a sport, walking, or swimming. You may be encouraged to exercise in water for low-impact activity that is easier on your joints. Additionally, a physical therapist may design an exercise program that strengthens specific muscles around your joints to help with your mobility.
Living with the disease
Living with spondyloarthritis requires treating the symptoms and avoiding triggers that may aggravate the disease. If you have spondyloarthritis, you should exercise regularly to maintain good joint and heart heath. You should not smoke, especially since smoking can intensify symptoms and speed up the rate of spinal fusion in AS patients. If you have spondyloarthritis, with some planning and guidance from your physician, you can manage your symptoms and lead a productive, healthy life.
Author: Gil Gomez, DO | Columbus, Georgia
Last edited on February 14, 2023