
Take a moment to envision yourself as a young athlete. You are pushing yourself to run faster, jump higher, and compete harder, only to be hindered by a pain in your knee. Every athlete knows the feeling of post-hustle fatigue, but when the knee pain lingers, it might be more than just soreness. For many growing teens, it is Osgood-Schlatter disease.
What causes Osgood-Schlatter disease?
 Osgood-Schlatter disease is an overuse injury that primarily affects young, growing athletes playing a sport that involves of a lot of running and jumping. The disease often appears in children between the ages of 10 and 15 during periods of rapid growth.
Osgood-Schlatter disease is an overuse injury that primarily affects young, growing athletes playing a sport that involves of a lot of running and jumping. The disease often appears in children between the ages of 10 and 15 during periods of rapid growth.
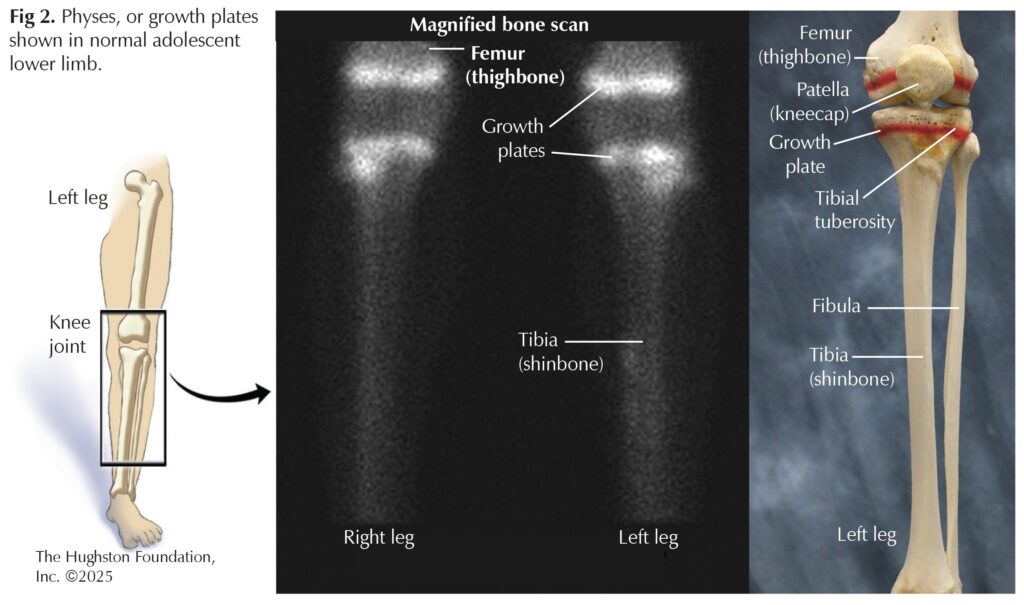
As children are developing, their bones are not as strong as mature adult bones, which makes them more vulnerable to injury.¹ Physes, or growth plates, have soft areas of cartilage cells that play a key role in the growth and development of long bones. After the growth plates have done their job, and children finish growing, the growth plates fuse into strong, solid bone.
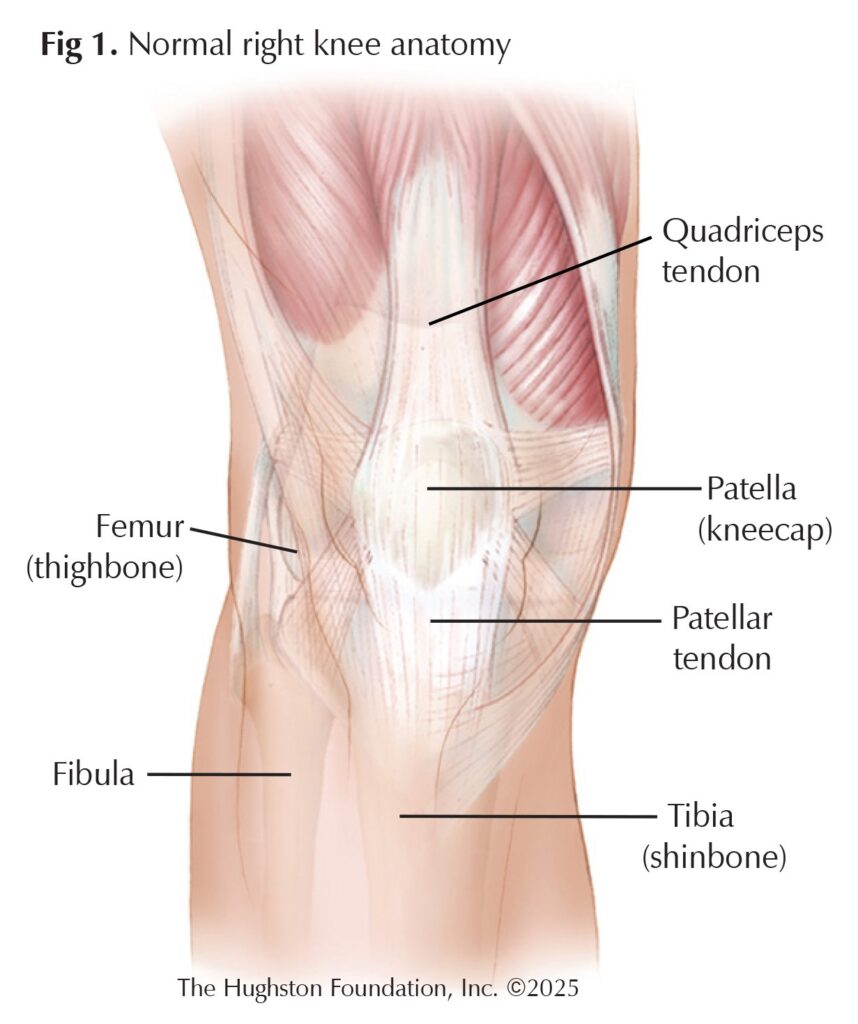
The patellar tendon connects the kneecap (patella) to the shinbone (tibia) and attaches to the tibial tuberosity (the bump of the shinbone just below the knee) (Fig. 1). When children perform movements like running or jumping, the quadriceps muscles contract, pulling on the patellar tendon, and tugs on the tibial tuberosity, which is located over a growth plate. Performing these movements repeatedly places a lot of stress on the knee. This continual stress can cause inflammation that irritates the growth plate, eventually leading to an overuse injury² (Fig.2).
Who is at risk?
Studies estimate the prevalence of Osgood-Schlatter in adolescents to be around 10%.2,3 The sport that the athlete is involved in also contributes to the development of the condition. Sports that consist of repetitive jumping, sprinting, and abrupt changes in direction impose a higher risk. Therefore, athletes who participate in sports like basketball, soccer, gymnastics, and track and field are particularly susceptible to Osgood-Schlatter disease.³ Aside from athletes, Osgood-Schlatter disease is commonly seen in boys, but girls can be affected too. For both sexes, symptoms often present during growth spurts, which tends to occur in boys ages 12 to 15, and in girls around 8 to 12 years old.²
Symptoms
Osgood-Schlatter disease can affect one knee or both knees. Patients often present with a dull ache, tenderness, and swelling below the kneecap. Since Osgood-Schlatter is an overuse injury that occurs due to an accumulation of stressors over time, patients may not be able to trace the onset of symptoms back to a specific injury or event. Kids with Osgood-Schlatter disease may begin limping or complaining of knee pain after a long day of physical activity or sports.2,3 As a result of the patellar tendon thickening, some individuals with Osgood-Schlatter may develop a prominent bump on the front of the knee. The bony prominence can persist into adulthood, but it should become pain-free after growing is complete.³
Seeing your doctor
If knee pain begins to interfere with the enjoyment of sports or other activities, it might be time to make an appointment with an orthopaedist. The good news is that diagnosing Osgood-Schlatter disease is simple and painless. During the appointment, the doctor will take the patient’s medical history, perform a physical exam, and possibly order radiographic imaging, such as an x-ray. When taking the medical history, the doctor may ask the patient to describe their symptoms and talk about their activity level or involvement in sports. When performing the physical exam, the doctor will take a good look at the knee and press on it to check for tenderness. The doctor may ask the patient to perform certain movements, like jumping or squatting, to see if it makes the pain worse. The doctor may order an x-ray to get a better look at the knee and rule out any other potential problems to confirm the diagnosis.²
Treatment
Hearing the word “disease” in a diagnosis can be anxiety inducing; however, Osgood-Schlatter disease is not something a child has to deal with forever. Symptoms subside soon after growing is finished and growth plates fuse. In the meantime, symptoms can be managed at home. Using cold therapy, like an ice pack, with over-the-counter anti-inflammatories, like ibuprofen, can reduce pain and swelling. Taking the time to thoroughly warm up and cool down before and after physical activity is a good idea too. Implementing stretching and strengthening exercises, paying extra attention to the quadriceps and hamstrings, into a daily routine can go a long way when it comes to managing symptoms. Some doctors may recommend visits with a physical therapist to help create a guided and more individualized plan. The doctor may prescribe an infrapatellar strap or kneepad that can protect the knee and provide support. Athletes dealing with Osgood-Schlatter should not push or play through the pain. Modifying physical activity or taking a break from sports is recommended until symptoms improve and become more tolerable.2,3,4
Prioritize your health
Osgood-Schlatter disease is not a one-way ticket to sit on the sidelines. With the right “game plan,” most young athletes can keep up with their active lifestyle. Recognizing symptoms early and taking the proper precautions to reduce stress and traction on the knee are fundamental. Thankfully, as children’s bones mature, pain and symptoms associated with Osgood-Schlatter disease go away. Understanding Osgood-Schlatter disease and teaching young athletes to prioritize their health is key to keeping them off the sidelines and competing pain-free.
Author: Claire Robinson, BS | Columbus, Georgia
References
- Anzilotti AW (Ed.). (2019 January). Growth plates (for parents) | nemours kidshealth. KidsHealth. https://kidshealth.org/en/parents/growth-plates.html.
- Smith JM, Varacallo MA. Osgood-Schlatter disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Updated August 4, 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441995/
- Corbi F, Matas S, Álvarez-Herms J, et al. Osgood-Schlatter disease: appearance, diagnosis and treatment: A narrative review. Healthcare (Basel). 2022;10(6):1011.
- Rathleff MS, Winiarski L, Krommes K, et a. Activity modification and knee strengthening for Osgood-Schlatter disease: A prospective cohort study. Orthop J Sports Med. 2020;8(4):2325967120911106.
Last edited on October 17, 2025